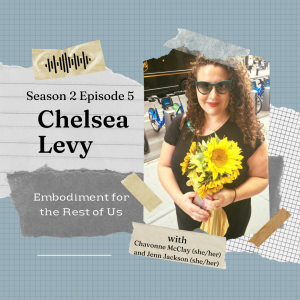
Embodiment for the Rest of Us – Season 2, Episode 5: Chelsea Levy
June 30, 2022
Chavonne (she/her) and Jenn (she/her) interviewed Chelsea Levy (she/her) about her embodiment journey. This is part 2, the encore, of our first-ever two-part episode!
Chelsea Levy (she/her) is a Certified Intuitive Eating Counselor and registered dietitian nutritionist. She earned her Master of Science from Hunter College and completed her dietetic internship at the City of New York (CUNY) School of Public Health. Chelsea utilizes Health at Every Size® (HAES®) principles in her approach to nutrition therapy. She works with individuals struggling with disordered eating and eating disorders, with a focus on weight-inclusive medical nutrition therapy, body image healing, and Intuitive Eating. Chelsea has interest in treating individuals with diabetes, and polycystic ovary syndrome (PCOS) along with folks, who are in larger-bodies, and those who are transgender or non-binary. She believes it is vital to provide care relevant to an individual’s culture, ethnicity, and overall identities. Chelsea hosts a collaborative space for the exploration of food and body healing through creativity and compassion.
Instagram: @ChelseaLevyNutrition
Content Warning: discussion of privilege, discussion of diet culture, mention of mental health struggles, discussion of dissociation
A few highlights:
6:54: Chelsea discusses her understanding of “the rest of us”
11:04: Chelsea shares embodiment practices do you recommend for folks experiencing various stages of eating disorder recovery
41:36: Chelsea shares how she help clients tune into the nuance of their lived experiences
52:46: Chelsea discusses her take on IE, HAES® and AND
1:06:24: Chelsea shares her online eating support on IG
1:15:27: Chelsea discusses ways in which conversations about embodiment miss the mark by letting systems and those in power off the hook
1:24:49: Chelsea shares how listeners can make a difference based on this conversation
1:30:47: Chelsea discusses how to be found and what’s next for her
Links from this episode:
ASDAH’s response to Academy of Nutrition and Dietetics’ Evidence Analysis Library (1)
ASDAH’s response to Academy of Nutrition and Dietetics’ Evidence Analysis Library (2)
BIPOC Eating Disorder Conference
Food Insecurity and Eating Disorders
Health At Every Size® (HAES®) (especially the FAQ for the origin of the HAES® movement)
Stress and Digestion (2): (TW/CW for the second page and fatphobic suggestions)
Fat Positive and Fat Liberation Reading Recommendations Beyond HAES® lists from Nikki Haggett and Vinny Welsby
Here is some info about what went on since March of 2022 regarding HAES® and the book’s author: here, here, here, and here among others (with updates to some of those here and here).
Music: “Bees and Bumblebees (Abeilles et Bourdons), Op. 562” by Eugène Dédé through the Creative Commons License
Please follow us on social media:
Twitter: @embodimentus
Instagram: @embodimentfortherestofus
Captions
EFTROU Season 2 Episode 5 is 1 hour, 31 minutes, and 41 seconds long. (1:31:41)
[Music Plays]
[0:11]
Chavonne (C): Hello there! I’m Chavonne McClay (she/her).
Jenn (J): And I’m Jenn Jackson (she/her).
C: This is Season 2 of Embodiment for the Rest of Us. A podcast series exploring topics within the intersections that exist in fat liberation!
J: In this show, we interview professionals and those with lived experience alike to learn how they are affecting radical change and how we can all make this world a safer and more welcoming place for those living in larger bodies and those historically marginalized who should be centered, listened to, and supported.
C: Captions and content warnings are provided in the show notes for each episode, including specific time stamps, so that you can skip triggering content any time that feels supportive to you!
J: This podcast is a representation of our co-host and guest experiences and may not be reflective of yours. These conversations are not medical advice, and are not a substitute for mental health or nutrition support.
C: In addition, the conversations held here are not exhaustive in scope or depth. These topics, these perspectives are not complete and are always in process. These are just highlights! Just like posts on social media or any other podcast, this is just a glimpse.
J: We are always interested in any feedback on this process if something needs to be addressed. You can email us at listener@embodimentfortherestofus.com And now for today’s episode!
[1:42]
J: Welcome to Episode 5 of our second season of the Embodiment for the Rest of Us podcast. On today’s episode, we have an encore follow-up interview with the generous and inviting Chelsea Levy (she/her) in a continued conversation about her embodiment journey and nuanced perspective on relational healing and nourishment.
C: Chelsea is a Certified Intuitive Eating Counselor and registered dietitian nutritionist. She earned her Master of Science from Hunter College and completed her dietetic internship at the City of New York (CUNY) School of Public Health. Chelsea utilizes Health at Every Size® (HAES®) principles in her approach to nutrition therapy. She works with individuals struggling with disordered eating and eating disorders, with a focus on weight-inclusive medical nutrition therapy, body image healing, and Intuitive Eating.
J: Chelsea has interest in treating individuals with diabetes, and polycystic ovary syndrome (PCOS) along with folks, who are in larger-bodies, and those who are transgender or non-binary. She believes it is vital to provide care relevant to an individual’s culture, ethnicity, and overall identities. Chelsea hosts a collaborative space for the exploration of food and body healing through creativity and compassion.
C: You can find Chelsea at her website http://chelsealevynutrition.com and on IG @ChelseaLevyNutrition. Thank you so much for being here, listening, and holding space with us dear listeners! And now for today’s encore episode!
[3:21]
C: This second season has been full of distinction, and our first interview with Chelsea Levy (she/her), was no exception. Chels is joining us from Manhattan, New York City — to follow up on our powerful first conversation two months ago and to continue talking about embodiment. There are so many things to explore together in nuanced conversation. Let’s begin! How are you, the human being, doing today, Chelsea?
Chelsea (L): Hello, hello, I’m, I’m happy to be back. Thank you for having me here.
C: Hi!
J: Welcome back!
C: Yay!
L: Uh, my, my being is tired, really tired. And I was thinking a lot about, uhm, how much unlearning I’m doing as well as continuing to learn in my embodiment journey and where that lands around my energy which is…yeah, it’s a, it’s something to continue to look at.
J: Hmm.
L: Yeah, I wonder, just sort of thinking about anyone who’s gone through an education process that, uhm yeah, has you learning in a certain way that’s holding space for research that doesn’t consider all bodies. What do we do with that? Where do we go emotionally? How do we express that to ourselves to our clients? And how do we actually take the time and space to then go and unlearn that as we are working as professionals?
J: Oh, it’s hard. It is not easy.
C: No wonder you’re tired. Yeah, that’s a lot. That’s a lot.
L and C: [laughs]
L: Yeah, I’m also really excited and pumped about it and I get FOMO about like unlearning courses that are intersectional. I want to do them all, and, and I feel really enlivened by them and there’s only so many hours that you can be awake and get stuff done in the day. [laughs] So my being is sort of, I feel like Silly Putty that’s being like pulled in different directions. But it comes back together, you know.
J: I relate to that.
C: Good analogy, the Silly Putty, yeah. For sure, I can absolutely understand that.
J: Yes, exactly. I was going to say I relate. I feel pulled in a lot of directions. And learning and unlearning are both exhausting, and they feel like they counteract each other as they should. Uhm, and it takes a while for it to integrate the learning and the unlearning. I mean, it’s exhausting, so I’m, I’m just sitting in that exhaustion with you. I feel that today.
L: Yeah, and I’m, umm, just for those out there, ust throw those out there, it’s been, it’s been a tough couple of weeks, a couple of days politically. And I just you know collectively feel till the mourning and my love language is touch and hugs and if I could be with the two of you right now and give you a hug.
C: I would love that.
J: I’d give you one right back, yes. Exactly.
C: Hopefully one day in the future.
J: Well, we’re so glad to have you back, Chels. And uhm, we had such a powerful extended conversation last time I wanted to jump and just sit with one of those things and sort of get us going again. How does that feel?
L: I love it. Let’s do it.
[6:24]
J: So if we revisit the second half of our podcast name, the rest of us. I’m curious what that means to you today.
L: Yeah, uhm, Embodiment for the Rest of Us. It’s finding space to live in your body and hold space for your feelings for, for folks who are marginalized to me. For other people, wherever you are, whatever sort of representation you hold. Uhm, if you’re underrepresented or marginalized in any way, you don’t see yourself, it’s hard to embody yourself physically and emotionally, holding in the present moment. And, umm, thinking about that as, as how I hold that understanding of what it is, what, who are the rest of us are. Where, where you know, people of color or people in larger bodies, uhm, transgendered nonbinary people who’ve experienced intense trauma. You know, whether it’s poverty or abuse, that this other space is for you.
J: Uh, I think the word that I hear when you say that is welcome.
C: Oh yeah.
L: Ooh. Welcome and, you know, hold, hold as much space in your body that you can that feels safe. Because it’s a process to really fully [unintelligible] in a safe way when it has never been safe to be you.
J: And space in the world, I could hear that being expansive.
L: Yeah, I, you know, I think, the goal for me is where’s, where’s the most freedom for anyone to really feel that connection to themselves and others? The most to be present in whatever’s coming up in your life and for a lot of people, that, that’s not a safe place, and so I, I find it really important to hold things for those folks in the work that I do. And I continue to do my unlearning of where my privileges holds walls into creating more space for others. Where can I bring down those walls and step back and lift others up? Where can I lift myself up where I haven’t been able to? And, and where can we connect?
C: Since we are recording a few months later, has that definition changed for you in the last few months, or is it where you were sitting before when you talked about the rest of us, what do you think?
L: I think in a general sense, it’s the same, but it’s always growing. It’s getting more nuanced and, and, just where my blinders are and where, for myself and for others, you know, where can I be more expansive in my embodiment? Uhm, so that I can, yeah, be collected and gives space or take space.
J and C: Hmm.
L: Yeah, that feels different. I feel like I’m connecting myself in it in a more vulnerable way and maybe before it was like hearing, umm, on the outside looking in at embodiment. Which isn’t really embodiment [laughs] it’s the concept of embodiment. But I’m, I am, yeah I think I’m trying to like yeah step into that vulnerability as a practitioner, as a human being, for it all as much as I can.
C: Hmm, hmm, that makes sense, yeah.
J: Hmm. Thanks for asking it like that.
[11:04]
C: What embodiment practices do you recommend for folks experiencing various stages of eating disorder recovery? How does one’s sense of embodiment impact nourishment and digestion, especially in eating disorder recovery and one’s relationship with food and body? Also, what caveats or exit strategies do you offer to resist retraumatization or if any part of the process is overly stimulating?
L: Oh, these are such great questions and…
J: We like lighthearted, very simple ones. Can you tell?
C: Very short, very short.
[All laugh]
L: I love it. No, I love it. And it’s such a good question, because you know, I’m working with behavioral health and working on a multidisciplinary team. And so I do want to caveat that, as a dietitian in behavioral health, yeah, I’m holding space for, uhm, some deeper sort of trauma showing up than maybe your more maybe run of the mill nutrition counseling we would expect. And so I definitely lean into the expertise of my team to assess what is necessary and safe for my clients in terms of what level of embodiment they can go to. And with permission from this team after assessment, really holding that space for my clients within the realm of food and body image healing and that can look really individual and different for, for the person. For some, we have more access to the breath and if we can get to that breath. I love working with breath as I have studied yoga and pranayama breathwork and that brings you back into the body directly into that present moment. But often that is not a safe place for folks with eating disorders. Some who are trying to not feel their feelings or you know the sensations of digestion and eating. So, uhm, I sometimes think, it’s OK to distract from those sensations so that we can get food in and that is a form of sort of harm reduction in, in the process of getting to embodiment. Maybe we are going to have certain topics of conversation that are lighter while we’re eating versus if we’re not eating together in session, then we might have a deeper conversation where we can have really, really uncomfortable feelings in the body and hold space for them. For some it’s, it’s about, umm, you know, sensory details like, do I need a weighted blanket? Do I need to turn the lights dimmer? Do I need to turn on a fan or off? Uhm, yeah. How is the temperature? Do I need a layer, all of those pieces? And can I take up space in the room I’m in and be reminded of it, you know? Like let’s take a minute and can I stretch my arms out? And like how does it feel in my fingers? And paying attention to those things. If, if it feels OK, or it, it’s, it’s accepted, sort of letting the person I’m working with direct me into what sort of level of discomfort, they’re willing to go into. But again, caveat in…I’ve talked to the psychologist and the therapist on the team about what really is appropriate for this particular person. I’m trying to think if there’s anything else that would be pertinent to that. I love getting silly. If someone was willing to uhm…pets bringing pets into screen, playing music sometimes. I was doing interpretive dance before between our cuts on the podcast, instilling some silliness and levity. This is something that I would definitely get into with my clients. We’ll dance sometimes, we’ll get up and just shake it out. Sometimes we have nervous energy, we need to let it move through us. So yeah, sometimes it’s fluttering our lips, and, and sometimes it’s cursing. I don’t know, it depends. That also depends on the comfort level of the person. Do they enjoy expressing themselves through particular language that is, you know, maybe not as accepted in your typical conversations? That might feel like relief, you know? So we get really creative about ways to let things move through us. And in terms of like what foods we eat, that, that’s really individual to–into what type of, you know, diagnosis is this, how far along, in terms of how much nourishment, is this person getting already. If they have intensely gastric emptying called gastroparesis, we might avoid certain foods and, and in other cases we might have more flexibility. So it depends on the, on the person and, umm, also, what we’re working on in terms of challenges for some people. Uhm, eating starches and different types of carbohydrates is really safe, and for others it’s really scary. For some people, eating fruits is terrifying and others, uhm, it’s a really comfy thing to eat, eat a bowl of fruit. So it depends on, on the individual and what we’re working on.
C: Not knowing, even before you said the word harm reduction, umm, harm reduction was like flitting around in my head and–
J: Oh yes.
C: A few thoughts. That, that was the first one that came to mind, and then you said you like to add some levity, you know, add some humor and, I…we haven’t known each other very long, clearly, but that’s something that comes to mind always when I interact with you is that you somehow can ground people, but also make them feel lighter at the same time. I don’t know what word that is. Like, I don’t know how you’re like…this is what I think of grounding it, lower, but then levity, I don’t know. Anyway, but I think that that’s a really good skill that you have, umm, of creating the safe place where you can be either. Well, you can be both grounded and have some lightness to it. I really, really appreciate that for sure. There’s something else I was going to say and I forgot. So sorry, Jenn, if you wanted to say something.
J: I agree with that exactly. There is a tethering to groundedness while also being, it’s like a balloon on the string, but the string is somewhere.
C: Yes.
J: Right? You’re not just floating in the wind. The phrase that’s coming to mind for me was autonomous choice. I could hear how someone interacting with you has the ability to make choices. Yes, I want to try that with you. No, I don’t want to try that with you when it comes to a multidisciplinary team. It’s like let’s be careful with this client. Something like X might be pushing them too far. Let’s try to sit in a space where we’re not in that level of discomfort, but a different level that they can tolerate sit with, find the edges of without too much distress, that kind of thing. So it’s thinking about that autonomous choice. It like lights up a passionate fire in me to think about autonomous choice, especially in traditional eating disorder treatment, it’s often taken temporarily or extremely long term or somewhere in between. And I was just thinking about how I wasn’t hearing that and what you were saying and how beautiful that is to me, it’s a goal of mine as well. That it’s not clamping down and containing clients until they submit. But it’s more like how expansive can they be and what amount of expansiveness feels OK today? Like they’re allowed to have boundaries, they’re allowed to say no. They’re allowed to say I don’t know. I could hear all of that in what you were saying. So I was just like that makes me go, yes! This is a place where I’d like to sit. As I already know about you, Chelsea, but that was, that was just sitting with me.
L: Thank you to you both. I love, uhh, both remarks and the, the idea of bringing a groundedness and then levity at the same time, and the imagery of a balloon feels really on point and then autonomous choice, umm, is just the perfect term for it I, I really am not into trying to coerce people into choosing. Uh, you know, choosing a certain behavior that I know to be safe, if that’s not safe for them in their mind, you know, we have to get there on their timeline and I can give them the information about the harm and ultimately we have to take, take the time and space to get there together in that collaboration. Uhm, because I think forcing anyone into, uhh, particular behaviors around food in particular. It’s like we might be able to correct that temporarily, but that might come with a whole lot of baggage of harm, and it doesn’t really bring long term healing in terms of that, this behavior. So I want to show people that they have a choice in what they’re doing and that it’s safe to play with this space that may also be really scary and dangerous, but with a harm reduction model on the table.
J: Hmm. Hmm.
C: Yeah. One thing you said in our last episode–because I listened to it last night and into this morning–that I really like and I had thought about it when we listened to before but hadn’t implemented it, but I’ll definitely be doing it is like the idea of like, harm reduction. If you can’t take 5 deep breaths with me, how about one? Or can we practice it When you’re not feeling heightened so that you can maybe access that a little bit later. I think that’s a really kind and generous way to help encourage someone to tap into that self care. Uhm, that just was really, really helpful.
L: Yeah, yeah.
C: Absolutely, and I hadn’t even thought about how embodiment kind of, well, everything impacts your physical body, right? So, of course, embodiment impacts nourishment. That just feels really important to hone in on for me, too.
L: Something that just came to mind was, uhm, and I haven’t done any reading of this research, but I know that there’s research out there about how when you enjoy food, you absorb it better. And obviously there’s, you know, probably a continuum on that of, like, limitations to those sites of absorption. If there’s, I don’t know, like altered GI or something. But, but that makes so much sense to me because when we’re not enjoying things we might be clenching, umm, our, like, villi and GI tract might not have the expansiveness to absorb as much. So I have to look into this, but I, I do think that the idea of Pleasure Activism. I have the book here, but that’s it, which is not specifically about what we’re talking about, but I just love the idea.
J: But it also is.
C: But it is.
L: But I love the idea of leaning into pleasure, and if pleasure is not accessible, umm, I think neutrality is the place to start, is maybe the window into body image healing, but also into maybe getting to a place of enjoyment around food. And I, I just find it the most exciting thing to think about and like the, the idea of learning to enjoy food, but if you hadn’t before.
J: It, it’s exciting, it is. It’s getting to be a, more of a human being than you were able to be before, which is so amazing and all. I have an article, I’ll send it. We’ll have it in our show notes. You are less oxygenated when you’re in your stress response, right? If we think about the rest and digest–nervous system and the…I don’t remember how they term the other one, but it’s like fight or flight, probably some of the adrenaline based responses right when we’re sitting in those spaces. We don’t have oxygen for digestion. Our body is never going to prioritize it. So how can we move into that space? I love that. So there’s my nerdy answer. It’s about oxygen, we can’t digest without oxygen.
L and J: [laugh]
J: Nutrition is the process of digestion is something that I do not hear said enough in didactic programs for dietitians, by dietitians, it is the process. It’s not the nutrients in the food. Are those important for the process? Absolutely, but the answer like where we’re looking is a super dynamic biochemical process that’s completely unique to each person. And so when we can look at smaller systems inside of that, like, are they even oxygenated? Like if they’re not able to get oxygenated with us, that’s not going to be safe. It’s not going to work even if they eat the food. They’re not going to be able to digest it. They’re going to have an upset stomach, GI tract digestion. It’s not going to feel good. We’re not going to feel safe. So what I was just sitting with and thinking about is that, like autonomous choices, probably something I think I said that every single day. Autonomous choice, autonomous choice! [laughs] It’s so important to me that I’m not taking that from anyone. I name it, I explain it. I say how it might sit in this situation? Have I taken that from you, right? Where is the nuance for you, that, that sort of look? I was really thinking about that while you were talking. Like life in a human body is where oxygen is flowing, right? If we think about functional MRI, how we visualize I’m totally nerding out. As we think about functional MRI looking at the brain in real time, where does the blood, and therefore oxygen flow, like what’s getting lit up? What’s happening? Uhm, when there is a gate or a ceiling or something like that on being able to process something, food, information from outside the body. You know mental health is physical health. Mental pain is physical pain. How do those things get in the way? I was just sort of sitting, I think I have to do a journal topic on this ’cause it’s making me realize that I talk about this all the time, but I like don’t go quite this far with it and I want to sit with myself at this level, that like really, I…I say functional MRI ’cause we can imagine blood flowing to an area of our brain. So we can also imagine it flowing to an area of our digestion. That’s why nutrition is always about the process. It’s also like ideas, like when things can get like I better be careful and only have certain kinds of “healthy food” is actually a restrictive process, like it’s not just the opposite of getting what you need, it’s that blood flow and oxygen are restricted. I try to think about it in a, a body term like that, especially inside of a conversation like this about embodiment, because whether or not they want to be safe with us is very different than I feel safe, blood is flowing to safe areas, I can safely digest that’s very different from, from want right? It’s not a mental exercise, it’s a somatic, cell spot, right deep in our individual cells, kind of, uhm, practice. So there, I totally nerded out on that [laughs], but it made me think of so many things related to flow and oxygen and, and choices of flow too.
L: Yeah, I think we, we choose to overemphasize on the food and not the experience, the environment of the food so that we can actually break this down, digest it and absorb it. [unintelligible] Into our cells, into our bloodstream, that oxygen is flowing on [laughs] to all our organs and brain that makes a lot of sense and it’s all part of the journey of healing. I–when you were talking, I was starting to think about and this is just a whole other like nerd out moment but just the complications around digestion that happened with eating disorder clients, uhm, because of their microbiome being altered because of the hormones that are not produced enough in the brain. And you know, particularly like serotonin and, uhm, other, other hormones that might interact, so that complicates the process of digestion and absorption in…and then there’s that added stress response of trauma. It’s so complicated, so to find space, expansiveness, room to breathe, to find space to open up, and not clench your jaw to take a deep breath. These are powerful, you know, places to lean into self care, and uhm, it’s more than just I don’t know, you know, taking a breath, right? It’s, it’s really part of the whole. It’s part of the whole train moving along.
J: Hmm. Yeah, not just the cargo or not just the, not just the engine. I was going to say caboose, but that’s the wrong part of the engine.
[All laugh]
L: Yeah like we, we forget to breathe sometimes and we and well, it’s all connected ’cause everything is moving, nothing’s static, right? Everything is moving, we gotta keep connecting to this movement in the body. We, uh, so that we can thrive.
J: Hmm.
C: Hmm, it’s a diversion, but it will bring us right back–I was thinking we’ve had a lot of therapists on this podcast, so it’s really exciting to have another dietitian, so I could just watch you nerd out. I’m like, I have no idea what you’re saying, but it’s really interesting so I’m really, really excited to watch you two interact, like I just want to say that that’s just really fun for me. It’s really fun to be present and an honor to be a part of this conversation, even if I’m writing a lot of words now that I have to look up. [laughs]
L: [laughs] I’m glad, I’m glad, I’m, I love to nerd out with Jenn always.
J: We do it on a very constant basis.
[All laugh]
C: I love to listen, it’s great.
L: So, uhm, before we get back into any yeah questions you might have, I, I…on this topic and Jenn, you might have some things, I mean, you’re both welcome to add, but, Jenn, you might have some specific understanding around this, but the idea that, umm, in restriction, particularly in anorexia, there can be a heightened anxiety around carbohydrates. We know, we, we know this to be true around, uhh, about particular macro nutrients that one in particular seems to be really scary for this population, and what we know in the brain is that the more carbohydrates you eat, the higher your serotonin levels can be. Happy people eat carbohydrates, however. When you have lower serotonin levels, when you eat the carbs and it raises your serotonin. It can be overwhelming. It’s like turning on the lights from dim to bright, and that experience in the body can be really overwhelming. So when people talk about people with anorexia in particular talk about this experience, uhm, sometimes I think it’s just, makes like, oh you’re, you’re just afraid of carbs, you know you’ll get used to them. I mean, there’s also other complications like I had mentioned before around gastroparesis and delayed nutrients from the stomach that can make things even more comfortable around digestion and bloating. But, umm, that added sort of nuance of when I eat this food, I feel even, uhh, more intensity. I think we need to hold space for that with compassion because it is a process to, umm, acclimate to, getting those, uhh, serotonin levels high enough to eat enough carbohydrates regularly. I mean obviously it’s so complex, but like, I don’t know, it’s just something that I don’t think is talked about enough and like with clients directly to just say hey like this…you’re not going crazy, this is happening in your body. This is, we know, we understand this from a biochemistry level, we understand what’s happening a little bit and we can sit here with you through this discomfort if you’re willing.
J: Absolutely, holding space for clients where we are uncomfortable and they are uncomfortable even if we understand it’s uncomfortable to sit with someone who fears something that they desperately need. That’s just a hard space. Uhm…
L: Did you, Jenn, have any, anything specific like around the serotonin levels or…
J: Sure. [laughs] So we create most of our serotonin inside of our intestines.
L: Yeah.
J: It’s not just a functional communication tool. Hormonally for the brain, it’s created in the gut. We absolutely cannot create enough or keep it around, right. There’s words like tonicity, the tone of serotonin, how often we keep it around. Uhm, medication works on reuptaking it, right? Don’t get rid of it. Keep it going, keep going, but in the body with food we can ask for more serotonin to be generated and for it to stick around. So in other words, we feel the effects of that, that are in, like, a mood sense uplifting, even euphoric. But you were talking about like the light switch coming on, euphoria, just like empathy. I always think about these two words starting with E. I don’t know why it keeps me remembering them both. Euphoria can be an invitation for things to escalate too quickly for a client so it is retraumatizing. So it’s something to do steady and at the client’s pace and full of that patience and compassion and understanding that you were talking about. Umm, I am very open in my practice and talking with my clients about harm from other dietitians. I hold space for that harm from traditional treatment models, I hold space for that because they often involve them not having that autonomous choice that I mentioned earlier and also being pushed to the lights are on, and I have sensory overload and everything is too much, right? And so anything that feels like it holds space. I don’t keep information from my clients, I nerd out with my clients on a regular basis to whatever level feels OK for them. I have like sometimes for different kinds of information. I have tiers of how nerdy I’m going to get depending on what the current capacity is or what feels OK because I don’t want to keep things from clients and I really get that from you to Chelsea and you as well, umm, Chavonne. It’s, there’s a transparency level, that’s why I love having a podcast with Chavonne. There’s a transparency level to what is being offered, so the choice can actually be for other people. Do you want to listen to this podcast episode? Here’s what it’s going to contain, right? Here’s the content warning. Here’s a trigger warning. Do you want to hear more about this information? Here’s what it might be about and what it might feel like. How do you feel now that I’ve shared that with you? Do you want to continue? And like we can stop those conversations at any time. There’s no rush, we can talk about it next time. Things don’t have to be on our time, that’s what I mean about the traditional treatment model. And with the way dietitians are usually taught in a didactic way in their internship, and also in practice through continuing education. We don’t have to go so fast. I think that’s something that I’m sitting with right now from what you asked and what you shared, we don’t have to go so fast, we can name that something is hard. You know in our larger culture there is a naming of like, oh, they’re overreacting, right? Major events in the news. Being in a pandemic in an ongoing way. That there’s an idea that there could be any kind of overreaction is absolutely ridiculous to my mind. Like how are we even functioning at any level, much less optimal levels, right? Like how are we even functioning? I have no idea how I continue to function. I don’t know how my clients continue to function, right? Like how are we continuing to function? It gets harder over time, so there may even meet a need for more ease and gentleness over time, not less, like there’s like this kind of idea that like once they get nourished to a certain point, they should be able to handle this. And now I can really go at them with the stuff they have to do, but I just want to sit with gentleness. OK, off my soapbox. I got really passionate and soapboxy.
C: I loved it.
L: It was great.
J: Thank you. Like meet people where they are today. Even if they are in a different place than last time. And even if next time it’s different, it’s waves, right? Life is waves. Let’s ride them with clients.
L: And where’s like, who says like this, where is that heading? Where did it come from, right?
J: Toxic people! Anyway, that’s my guess.
[All laugh]
J: Actually, this really relates to the next question. Does that feel OK for me to transition, or am I skipping over anything?
C: Can I say one quick thing?
J: Of course!
C: I’ve got, it’s just a quick little “boop”. One thing I was sitting with as you two were talking. In addition to just watching you and loving watching you nerd out, it just shows how important multidisciplinary work is like, uhm? Uhm, you can do the, the nerding out: this is why this is happening to your body with the serotonin. Well, and then the therapist can be the one that handles the what’s happening to your body on an emotional level if you’re incorporating these carbohydrates. It’s just, really it just, it’s really makes me really grateful for multidisciplinary teams that exist and people who are able to access that care so you can get help, you can get support from different facets and different people, have different knowledge about the same thing to make sure it’s a more encompassing view. I think that’s great, I mean, it’s really great.
L: I love multidisciplinary teams and I believe that we would benefit if they existed across like all medicine, not just in behavioral health. And you know, yeah, we would all benefit from that.
C: Absolutely.
J: Yes yes yes yes. Uhm, and it also is like highlighting for me and sitting for my clients who are not able to access a multidisciplinary team. How much of the burden of knowledge processing integration? How am I emotionally, right? All those sorts of things fall on them, right? It makes recovery, recovering, coping. It makes things continually retraumatizing right? It’s, it’s, it’s hard. It can still be harm reductive, but the reduction in harm is far, far less than if they’re going to multiple spaces and hearing similar things. Then, then, then, if the team is able to communicate and they say, well, I heard you talked about this, is it OK to talk about that in here ’cause that seemed really important to you, right? Inviting a conversation to be continual because it is. And making that easier, it’s just more relational, right? Where the relationship is different with each practitioner with any client or patient when there are other practitioners. There’s a depth that can be reached.
C: Absolutely.
J: Umm, that’s, I notice that all the time there’s a difference in the depth. Makes me sad every time I think or say that, umm, that the depth can’t always be there when someone doesn’t have access which is not their fault. They didn’t do anything to make that happen. That’s just the, what they’ve been handed, right? And even the idea of pursuing that when they don’t have access is just another burden on them. I mean, it’s, it makes it harder. It’s why talking about food insecurity like are you hungry most of the time? Growing up, did you have access to food? Where those conversations are so important inside of an eating disorder conversation or before one, right? Because they’re, they’re so…I think a stat I heard last week, it’s, it’s at least over half. I think it was 60% of people who are accessing a food bank, a food pantry, something like that have some recognizable eating disorder symptoms, like it’s just, it’s sad, so and it’s, uh, I’m so grateful for being on a multidisciplinary team when I can be. Uhm, I don’t want to over shadow how hard it is for the practitioner, but I also want to emphasize that it is the hardest on the person going through the eating disorder, recovery and coping rates. And that’s what I meant. I think this also was like it’s an uncomfortable space to hold like I’m just kind of sitting in that uncomfortable spot, right? Now it’s hard to hold those things. And, and to and to normalize that. You can still go at your own pace, even if you don’t have the same access as other people, I think, is also really important. They don’t get to see that in other people. Uhm, that they get to have space held for them at their own pace. But they also don’t see some of the harm inside of eating disorder treatment, I guess either, but what I’m really thinking about is it’s hard to know what your pace should be if you don’t have someone to bounce it off of in a context, that’s so hard and so new. So more soapboxing and nerding out. [laughs] I could do it all day, you know I could. And this also like the, the question Chavonne, uhh, questions Chavonne’s asking, the questions I’m about to ask, feel very related to me because it’s like leaning into that depth, space that I was just referring to.
[41:36]
J: So something you and I talk about a lot, Chelsea, is that bodies are complex biochemistry, this complex, umm, clinical experience is only one part of what’s important, evidence based is only one part of what’s important and lived experience, a client’s lived experience is incredibly important. Uhm, and we only get highlights snapshots of what’s going on, right? Whatever they choose to tell us. So how do you help support clients to tune into the nuances of their lived experiences? And I’m just gonna throw some words out there that I was thinking about that these words can be around, but it’s really wherever your brain wants to go: coping, recovery, aging, chronic illness and pain, mental health and needs and just being a human being with a body.
L: Umm, thanks.
J: Another light question from me. [laughs]
C: Very short.
L: I really resonate all, they resonate and sort of are incorporated in different ways into spaces that I hold with my clients and I think it’s an autonomous choice, it’s that permission, asking for permission, staying in a space where I’m asking questions with permission. I’ve gained trust and I can ask questions that I think are important for harm reduction around the level of motivation that might be there, what’s not being said in the room that feels really important to talk about that’s been mentioned before, or I know as a goal or you know what goals might we need to reassess and bring in to consider together to focus on? I mean, of course I want to hold space for whatever the client wants to talk about in this, in the time there with me, and of course the lens of nutrition and body image. Umm, and it can show up in all kinds of ways about maybe we’re, maybe we’re stressed at work, or maybe it’s something relational with a partner, umm, or maybe it’s something internalized that we’re like working on in our therapy, or it’s something with pharmacology that’s being changed, and so there’s barriers to meeting goals that we’re working on. And so it’s always really about where there’s more space, where can there be more time and space to hold? To make more room for healing. I know that sounds super like mushy and cliche in general, maybe?
J: Not to me.
C: I liked it. I liked it a lot. [laughs]
L: Oh, thank you. Thank you. But I mean that you know, like I think, sometimes people come in with this like human doing instead of human being, perfectionistic capitalistic, way. And I want to honor the whole person and slow down and check in with what we’re working on and find more space to stretch our motivation, our level of motivation maybe. So it might be for five minutes and we might talk about something totally different for the session, but for five minutes we can hold space or something really hard and important that needs to come up. And there’s space for it and that and that’s growth. You know, it depends on what’s going on in other, other times, it’s very technical and like I need, I need help figuring out like, I just don’t like the way anything tastes and I need to figure out what to eat. Like, what’s the plan? What to wear? Uhm what I like, yeah, like what do I do with how I feel in my body and showing up around other people? And you know they keep going, all kinds of directions.
C: Yeah, umm, so it’s really just a lot of holding space, whatever feels, I was going to say pressing, but that’s not the right word, but whatever it feels like it needs to be in the room at the moment.
L: Yeah, yeah, and that’s where I think harm reduction really is always being held.
C: Mm-hmm. Absolutely.
J: Yes, it can be agendaless while also still having structure and a direction. Uhm, I mean agendaless on our part. I mean, obviously I always say agendaless and my brain like fills in an agenda, so that’s what just happened for me. But there’s like, I mean, like we can name why we’re here, together, right? Are we going, we’re going towards the same place together, but I just mean a separate and distinct agenda. The coercion you were talking about earlier is, the what I mean by agenda, sitting in a space free from that harm reduction sometimes is someone needs to be listened to for a session about whatever is on their mind. Uhm food, body, body image, it doesn’t really matter, they just needed space held, right? That’s also, uhm, to have to show up and perform with a dietician with a therapist, with another member of a multidisciplinary team can be the opposite of harm reduction. Yeah, it could be harmful, so I was just thinking and sitting with, after Chavonne was reflecting like how’s the space holding where there isn’t judgment, right? Human beings judge, but I mean purposely holding a space without judgment with patients, with compassion, and where clients cannot disappoint us. Something I think about a lot with traditional eating disorder treatment is how disappointed professionals are with their clients and patients, health professionals. There is so much disappointment directed at patients that they say the fear and shame of that is so constant. I don’t want to be a part of that, so I guess I’m just sitting with I, I want…you’re helping like reinforce or helping me remember and recognize that I want to clearly state and have clients know that I’m there. They can’t disappoint me. They can come with anything and it will be received. Maybe an exception, right? We can find space for that.
C: Yeah, and I think you have to be really intentional as a helping professional, because eating disorders, eating food, body image, etc are so fraught with all of these societal “norms”, these societal expectations so there has to be really intentional space. There is no judgment. There is no disappointment here because I feel…I, I’m not going to speak for dietitians, but at least as therapists, people who are coming in for help and support are so…they already feel like they’re doing wrong, and that’s the last thing they need is for another person who’s like this is what you’re doing wrong. So it’s just, it’s, it’s a really intentional space that we have to hold, I think, in, in terms of eating disorders.
J: Ooh, to riff off that, Chavonne, you’re helping me realize that there is a specific harm that happens when we’re disappointed and we collude with their eating disorder.
C: Mm-hmm, absolutely.
J: That’s something I’m always trying to not do, but I’m just realizing how easily directed we are in that direction. When we hold disappointment, and when we hold judgment, and we point it at clients. It’s, you know, not every dietician like me is willing to say, I get there are things that are harmful by other dietitians. I have to undo some things, I have to invite them to another way, because something has colluded with their eating disorder, like they learn things in some traditional treatment models and with, uhm, so sitting in a harm reductive space is sometimes sitting with that part as well. That makes me really itchy and uncomfortable to say out loud, but I sit with it all the time. I actually can’t think of a single exception to that, so it’s, it’s a hard space, but it’s important that, that the safety is not conditional. And that there isn’t an alignment on our side with the judgment and disappointment of other people, either. I’m going like hard and fast at this. [laughs]
L: No, I mean there’s so much harm out there and yeah, you know, I try to do my best to navigate people away from harm if I can help it. And as humans I know that I’m unintentionally going to harm people just by doing what we do, by talking, and maybe there’s something internalized that there’s trauma that I don’t understand or know about that is being activated and that’s happening in our, in our space is, uhm, held space so that it can be maybe looked at closer with the therapist on the team and, and worked on for more healing. But yeah, I’m always holding space for there’s no failing. I have a client who wants to get an A every week, she says did I get an A? And I, and I say there’s no grades, there are no grades here because really, there’s, there’s no, umm, there’s just no right or wrong way to do any of this? And I would say the only thing is just, there’s harm, like we want to try to avoid harm where we can, you know.
J: Yeah, I’m sitting with how red my face has become and that I feel it being noticeably hot. There’s nothing that riles me up more than, than someone else causing harm to a client of mine and that they, that they still feel shame and fear from the stigma that was sent in their direction.
L: Yeah.
J: I mean, that they’re trying, you know, clients work so, so, so, so, so hard at healing when, when they’re given ideas to work so, so hard and it begins counteracting that, it’s just, it makes me angry, right? And I can hold space for those human beings who did that harm and still not want it done to my clients. So I’m sort of sitting with both, but it sure lights a fire under me with my like see through skin. [laughs] It’s just like nothing but redness that I’m seeing now which just sounds like a match for how I feel in my body. [laughs][52:46]
C: Umm, our next question, we’re curious about what your take is on Intuitive Eating and/or Health At Every Size or HAES and the current state of those modalities and conversations, especially considering the events of the last couple of months with the Academy of Nutrition and Dietetics Evidence Analysis Library and the HAES book’s author and harm of fat Black, Brown, Indigenous and People Of Color. Where do you think they fall short and how can they be expanded? Another easy, light question.
J: We’re real light today.
[All laugh]
C: Next, we’ll ask your favorite color. It’ll be fine.
[All laugh]
J: You know ours, there are headphones for those listening, she can see us, our favorite colors.
C: Purple and blue, always!
L: Yeah, I mean, there’s been so much going on and I think it, it’s really needed to happen, it’s indicative of the fact that a lot of people, I think, thought that the author had come up with HAES and was the originator which in fact they weren’t, so there’s like course correction here that has needed to happen, to go back to the roots of Health At Every Size. To really honor the most marginalized and hold more space for marginalized larger BIPOC folks to really be center stage and re, rewrite the book, really. I mean that’s, I’m excited, I’m, I get like, I’m getting tingly thinking about that book to come, you know? And, and there are organizations that are coming together to, I think, take the next steps and what that could look like. So that feels really important in terms of the Academy I just…le sigh. I’m never shocked about the level of disappointment that I, uh, experienced by witnessing, yeah, how much weight stigmatizing data they put out there. And you know some, some things I think about are that the folks that are on those boards, holding positions that are voted in are not there for very long, so in some ways that feels cozy. You’re like, oh, like I, I’m not aligned with what you’ve put out there. That’s weight stigmatizing and you’re not going to be here in two years. But it continuously is being centered around thin, white people in the research in, umm, in the library, in the EAL. And even though there was pushback on that, nothing came of it. So, it’s like, do you really support these organizations? I think buying power is where our power is, umm, as a collective of people like where, where can we make waves? We can protest, we can, uhm, petition we can send in surveys to the board. We can let them know and communicate all we want. I think the loudest communication is, is how we spend our dollars and cents, and so you know, it’s like, hey, if you’re not going to consider me, why should I be part of this community? I don’t, I don’t need you to hold the credential, so if you want my money and my, my time, maybe maybe, you’ll consider me in your decisions. So that’s sort of where I stand on that. And I think change is hard. I think you know when people get dismantled and are brought in it’s uncomfortable but necessary. And so, uhm, we’re gonna see some, I think waves, in terms of just like who, who are we going to center? Umm, somebody who was privileged and educated held all of that power and went around to conferences with their book? And I think you know it, it’s their time to support other people and lift other voices who they really leaned into to be where they are today. So I hope that happens and I plan to put my dollars and cents toward the people who are marginalized who should be centered, in my opinion. You, uhh, know that’s really where, what it comes down to. I said that without [unintelligible]
J: I appreciated that.
C: No, that is great. That is great so we don’t center certain people, that’s fantastic. And, but I think that’s exactly what it comes down to, putting your dollars and cents, not yours specifically. My dollars, you know in the general your. The collective, yeah, the collective, your dollars and cents of where it belongs. To center those voices that are the most marginalized to enable them to continue to, as I was going to say, continue to speak their truth. That also sounds like that’s asking for a lot of labor, so that’s not exactly what I mean. But, umm, I agree with you, I’m just not finding the right word right now, completely.
L: It feels a little like shaky right now. Like where are we, as a, as a group, as a cohort? In dietetics, you know we’re the minority, Health At Every Size, or Intuitive Eating or…although they’ve become more popularized, they’re not centered in the training, and they’re, they’re not the majority. I would, you know they’re, they’re the minority and so now that we don’t have like a leader [laughs] Uhm, well, I’d like multiple people to have platforms, but we’re in such a transition so it feels a little unsteady. Like where do we go? Where do we refer to? People who are learning or stepping into this space for the first time? So the part of me that is uncomfortable, wants it to be solidified. But you, you know, in that interim, I’m also grateful for the shift because it is really necessary and important. And I want it, uhh, I just wish it was like, like I said, solidified already like we had the book, we had the group, like you know, like it was done and like I could get more people on our team that aren’t are maybe more in the weight centric paradigm, or you know. Yeah, but that’s OK, right?
J: Yeah, there’s a lot of itchy, sticky, sweaty nuance.
[All unintelligible]
J: I’ve been scratching my legs, it makes me itchy. You know, I’ve actually, I’ve been sitting, I’ve been sitting in that same space. And a client asked me this week, what are we supposed to do now? It’s the first time I was directly asked and I chose to try to answer and I was just remembering my answer as you were saying it. And I’m going to say it again now because I’m realizing how much I like that I didn’t have to like create some sort of like talking points to get myself to come to this. It was just more from the heart. Uhm, there’s nothing wrong with Health At Every Size. Its origins are from people of color, from fat activists, Black people specifically and it didn’t start with the author of that book.
L: Black fat lesbians.
J: Yes, yes, sorry it started with fat, Black lesbians who were [unintelligble], pioneers.
J: Yes, thank you, thank you. And, and so we can honor that by doing all sorts of things, we can listen to fat activists, we can get that body… So in our interview with Lindley Ashline earlier in the season, I love their definitions of body liberation and fat liberation, right? We can actually acknowledge and normalize experiences in all bodies. The, the fattest of bodies, right, disabled bodies. We can normalize these experiences. Uhm, we can also hold a space where the most marginalized are centered in that conversation. So Lindley has that as fat liberation. I’ve been thinking about that, so I chose to say that to my client. It felt really, it made me itchy. I wasn’t sure what’s gonna happen. It’s–I, I felt like they were OK in their point in recovery for me to say something like that. You know, all of that stuff I’m gonna turn into a really beautiful conversation of thank you, I didn’t know where to look, so I think something that is important is that clients don’t know where to, what I used to look at this book. I used to look at these people. Where do I look? ASDAH has a wonderful link to the history of HEalth at Every Size that includes this information, uhm, yeah, yeah, they’re doing a good job. There are an incredible number of books, and we’ll put these in the show notes. Again, we did at the end of last season, but we’re going to do it again, which is Nikki Haggett. Oh my gosh, I can’t remember the, the name of the other person with…
C: Vinny Welsby.
J: Yes, thank you. So Fierce Fatty is their handle on most platforms. They talked about all the books that actually are talking about this and have been talking about this and continue to be published and talking and talk about this, not centering the person who wrote the Health At Every Size book, right? Like there are so many options, so it’s like those two lists are people, places to send people and just in general, following fat liberationist and fat activists, right? These might not be people with credentials that might not be people with the fancy PhD who have “researched” the “evidence based”, right? These are people with lived experience who have been talking about this for so, so long, right? It’s just up to us to listen and, and I think that orientation, umm, towards liberation is really important, because that’s supposed to be the intention of Health At Every Size, towards liberation. How liberated can this get right? Some limits, it’s still inside the medical industrial complex, but how close can we get? So sometimes I think that this opportunity is to look beyond Health At Every Size as well, which are some of these other things that I’m referencing.
L: I, I love what you’re putting out there, Jenn, and I couldn’t agree more that when people ask me for resources, it, it is more sort of grassroots and individual and the thing that I’m really itching for is something solidified. That’s cohesive to send people to that streamlined, but there’s there, there are a plethora of incredible folks out there who have been writing and speaking about these topics for years and years and years and with the Internet we have access to them, so supporting them is, is the interim way to and continuously but until we have like one place to send people to as a streamlined flat platform, there are many different places to go, and in fact that might make more sense for someone who’s looking for a particular voice that speaks to them.
J: Mmm. Oh, well said, yes.
C: You know, yes, that’s a really positive reframe for someone who’s like, I want one place it’s like no, now you can look at all these other ones and see which voice really speaks to you, that’s a really positive way of looking at it for sure.
J: Autonomous choice even in the voices that you listen to.
L: I, yeah, I love that. When people, yeah, are asking me for resources around a particular book on a topic, I often will send a link to a podcast from an author or someone who this is, you know, an authority on a topic and, and so that can give you access to yeah, just sort of the heart of it, and then you can dig deeper if you feel inclined.
C: Absolutely yeah, completely agree.
J: I appreciated that reframe and these were…I’m going to use the word I always use, expansive, ’cause it’s feeling, has been feeling really contained. That’s what made me think of the client is that it can just feel so contained and to go in whatever direction is not the most containment, feels, harm reductive on a much larger scale and sense.
[1:06:24]
J: Umm, you host an eating support Instagram live through your account which is at Chelsea Levy Nutrition with–and Chavonne and I have both been on there. Can you describe that space and how you–something that I think is so beautiful. So I want to ask about it is, how you cultivate embodiment virtually, connection, embodiment virtually with those seeking eating support while recovering from an eating disorder.
L: I love that space and it’s been lately a little less, most recently just out of being a little burnt out, but that will pick up again and in the past several I would say couple of years now we’ve been meeting every week, which is pretty wild and now maybe one or two times a month. But in that space, uhm, people are coming from all around the world and know each other a little bit in the comment section. Uhm, cheering people on the community and connection is really powerful. It’s, it’s palpable and, uh, I think it’s about being human, like just showing up and being real and, uhm, you know, I try to center, umm, guests who are marginalized, as my guests to lift their lift them and their voice and showcase them to folks who are in need and use that space in a way. Like I, I do with all things, I try to bring a grounded space with levity, and so you know, uhm, every week has been different, but sometimes we play games, sometimes we uhm, I don’t know, it depends on the person who’s come onto the, the interview space, but I might center them and what they are offering in the topic. But then really, it’s just whatever is going on in people’s lives, and knowing that they matter and showing a little piece of myself and my life and eating too. And knowing that, I think, I think something collective about this is that you know, people come into healing spaces. You know they’re…whatever is going on for them is happening to them and you’re holding space for it but this is, this pandemic is happening to all of us, clinicians and clients alike. And so holding space has been really meaningful for me to, to just connect with people out there when we couldn’t be around each other, so I think that is why it’s been so powerful because it has so much meaning.
J: That makes sense.
C: Mm-hmm, it’s really great for people, especially who live by themselves or are home by themselves a little more often than other people to have someone that they can eat with. I think it’s just really, it’s really, really nice. It’s a really great space. Thank you for creating it, for cultivating that.
L: Thank you, umm, and I try to let people know, you know, whatever it is. Is, is it hard to decide what you’re going to make? Maybe you want to tune in while you’re cooking something for yourself or picking something up or ordering in, or maybe you want to sit with me after you’ve eaten and you just want to hold space and not be alone with digestion and that discomfort of bloating, whatever it might be. Maybe you aren’t struggling with eating, but you just are really lonely and you want connection, this place is for you.
J: Yeah, it’s a place for people who eat, which means it’s a place for people, yeah?
C: Oh, I love that. I love that.
J: It’s so simple, I’m just sitting with the simplicity of it and also like wow, I know it that we’re two years into a pandemic, but I didn’t really think about eating support also being for the same period of time, right? Like within one month. Uhm, so it’s just like pretty wow and, and people who have been coming that whole time, some of that time. I, I personally try to go when I can. We can all use different forms of connection in, in the pandemic, and it always surprises me how connected we can be virtually. And so I think, it’s like, it’s like the tethers between us. Like I’m showing myself [laughs] reaching for these two on the video for those listening. But right, there’s like these tethers between us, and we could be grounded on our side with food, the experience of digestion, taking care of ourselves in other ways, preparing food, whatever is showing up, I just think, it’s really beautiful in its simplicity. Uhm, something that I still do that things like that remind me of is, you know, eating disorder work as a clinician can be very complex. We’ve talked about some of that today, but being a person and being a person who eats is not very complex. Sometimes, like sitting with, how to make something is really important. That happens to be an area that we learned way more about recipes and foodservice things than I would have liked to know, but it does give me information like the food aspect, loving food, cooking food, interacting with food. Uhm, just sitting in a place where you can get ideas you can feel really stuck. It’s just a place for not being stuck. Or being stuck, but the room is moving so it doesn’t feel like you’re as stuck or any sort of thing like that. It’s not just expansive, it’s not just simple. It has a real direction to it, uhm, that’s like towards people, so towards embodiment. It’s also like even if it’s staying still, it’s still pointed in a forward direction. I don’t know quite how to say that, but there’s always something really beautiful there about how people show up for each other in the comments and, and also how, as you were talking about how it’s different every time, that’s very true, but it’s always supportive, yeah? So that’s a hard thing to continue for two years and have it still feel that way, and in fact I would say that feeling there has grown.
L: Thank you. That’s beautiful.
J: So that really speaks to the kind of space that you hold and continually hold and expand as well. Just to fangirl about my friend Chelsea for a minute.
L: I love it, that’s really meaningful to me and I really want to do more of them. I think the most challenging part for me is to like take the energy to book people to come. But I would do them every week if somebody was like I’m ready to go, so I will be putting that energy out there.
J: We’re ready to go!
C: Yeah. I eat.
[all laugh]
C: I’m a person who eats.
L: I love that, you eat, you wanna eat with me live? You know.
[All laugh]
L: It’s that simple, easy as that.
C: One thing I actually really liked about it being a guest. It was super exciting. I was actually kind of nervous, I don’t…well, it was my first time doing something like that, but when I, when I have been able to tune in, it reminds…I, I’m not personally a person who forgets to eat, but I don’t always eat at the most structured times. It was nice to be like this is the time that you are going to stop what you were doing. ’cause I think so many people are transitioning into or have transitioned into being at home. It’s easy to get pulled into all this stuff, so even if that wasn’t something that was discussed during it, I really appreciated that structure around it too. Not in a diety of way, but just like oh, I should eat. I should, I should eat.
J: You know, as I was, as I was listening, uhh, to you say that, right? We’re people who eat and we live in a productivity culture. We live in a purity culture or even a perfectionist culture. It’s hard to eat. I want to like normalize it for every human being. It’s hard to eat amongst all that shit. It’s hard to even–you don’t have it in your schedule. You know one eating support session can be an anchor for an entire month, that’s actually something I’ve seen evolved in the comments. But it’s like, remember earlier this month we said this, well, this is happening for me. And there’s these beautiful, continued conversations you know on Instagram Live as you and a guest are the ones who everyone can hear and see audibly and everything else is happening in the comments there. Like, there’s like a little heart button, but that’s, that’s about it, you can pin one thing that’s it. Uhm, but for it to be so dynamic, uhm, and interactive also speaks to that space that you create. I just think it’s awesome.
C: Absolutely. Just, just wonderful.
J: Thanks for answering that. And I’m serious. I will come back anytime so you can consider that labor done.
C: Same.
L: Thank you, it’s an honor.
C: I will happily eat.
[All laugh]
L: Yeah, and eating is a form of embodiment.
J: Eat and talk. I love you, Chavonne.
C: Love you, too. Sorry, getting the giggles. [laughs][1:15:27]
C: For our next question, what are ways in which conversations about embodiment, body image and health and wellness missed the mark by letting systems or those in power, especially those with credentials off the hook? Like very, very light.
[All laugh]
J: I’m really sitting with how hard hitting this is today.
C: But there’s something about you Chelsea that just like, yeah, I mean, I love the surfacey stuff too, but I’malways like let’s just do this, let’s just get in there and just mix it up. I–something about your energy really brings that to the front and I love that.
L: For those out there who are into it, I’m a Capricorn, which is another sign that might have something to do with it.
C: Ah, I don’t know enough about Capricorns. I have to read.
J: Oh it does. I got a, I have a Capricorn moon and it–just totally got what you said.
L: So yeah, like how are folks getting out of this…umm, can you read the question one more time? I just wanna like let it roll through my head.
C: Of course. What are ways in which conversations about embodiment, body image and health and wellness missed the mark by letting systems or those in power, especially those with credentials off the hook?
L: So I think because we come from a weight-centric medical model, they, they being folks with credentials, get off the hook because they get permission from, with their power from their credentials, and from the sources that they learn from. Uhm, they are receiving harm, right? They’re receiving, umm, information that is in fact unethical around dietetics, and I can’t speak for other disciplines, but I, I, I know, I, I mean, I can’t speak for like true med school, because it’s a weight centric medical model. And we know from research that’s been around for several decades now that intentional weight loss, uhh, is not sustainable, and that shift causes weight cycling in, in its promotion,. So uh, folks with credentials who are trying to, I don’t know, promote some sort of wellness and embodiment around, uhm, the idea that you can just change your size are causing harm through weight cycling cardiovascularly. And then, you know, I think it’s about folks who have credentials who are trying to do good but not centering the people that need to be centered. That’s really where I’m seeing a lot of the body positivity movement going, being co-opted by providers that are straight sized and not marginalized and I, I think that they could do a better job in the way that they communicate and lift others who have had more oppressed experiences in their life. That being said, we don’t have enough clinicians out there that are oppressed and marginalized because they are oppressed and marginalized.
C: yeah.
L: So it is like this, you know, like it’s really fucking hard. So, umm, but we all need to do better, including myself. And in my unlearning, I’ve learned that, like I, I can make space for more people, and so I try to do that in my own way, and then also center my lived experience being in a larger body and to the best of my ability, but I’m not a monolith and my experience isn’t someone else’s. Just that so, I, you know, yeah, sort of tread lightly on that one. But yeah, I mean those are like two sort of variables that I think about and, and the, the folks who aren’t even trying to unlearn. That’s just what really fucking sucks the most. I guess we need to keep, keep putting the education through and see where we can make waves and center, center more voices that need to be heard.
J: It’s making me think of Diversify Dietetics who’s actively trying to bring particularly Black dietitians into the field.
L: Yeah. Mm-hmm.
J: I’m thinking of Whitney Trotter’s BIPOC conference this summer in July, so about a month after this will be published. Uhm, and I’m also thinking of, also with Whitney Trotter, the BIPOC Eating Disorder Provider Registry, so like centering those who do exist, bringing new people in as well. And, and I, I’m just riffing off of you saying centering them, but I’m thinking some people have really created these resources. Just like with the HAES conversation, there are other resources, so definitely going to be in the show notes.
L: Yeah. I think that we have some great folks in our Health At Every Size space or body liberated space, uhh, that are already doing this and, and we need to be doing it more and more people need to know about it and utilize this resource. So I love that these links are going to be in the show notes. Whitney Trotter’s a great resource, Diversify Dietetics is a wonderful resource. Umm, yeah, we need, we need to see this across all disciplines.
C: Mm-hmm, absolutely yeah.
J: Let’s not get off the hook. I’d like to be on the hook and then I can tell that’s very much the conversation we’re having yeah, yeah.
C: Yes, and I think in addition to them being let off the hook, I think that this culture that we live in, where we glorify education…I mean, education is important. I don’t want to say it that way. But like, we, we put this education on a pedestal. We put these credentials on a pedestal. It’s not just these people who are being taught the wrong things. It’s also the fact that we are like, well, you have these credentials, so of course we’re going to listen to you must know everything more than everybody else. It’s learning the wrong shit and also glorifying the wrong shit. So yeah, I think that’s a big part of it.
L: And that comes back to like the unlearning, the learning to get the credential, the unlearning, that happens and and, and who’s doing it so that we can create, uhh, uhh, more diversity in our space. Or even the you know, white supremacy culture that teaches the, you have to get these credentials to even like talk about anything to even be a “success” in this American, I’m speaking about America because that’s where we are, American societies. So yeah, that’s really sitting with me, right now.
L: The, the idea that we all need to go to college and get it and get credentials. Uhm yeah, it really misses the mark. There’s so much more to society as a whole to embody. We, umm, what makes us most alive and how we can contribute to connection. A man doesn’t have to be one, one trajectory. Yes, and in this virtual world that, uhh, I hate saying benefit about the pandemic, but a bright light or a spot can be–
C: Silver lining.
J: Yeah. How we can get things virtual and not to take away from things. Silver lining but like let’s actually add something ’cause it all sucks and all that stuff that, that not, that’s not correcting you. That’s correcting me, where I was immediately going to, go with that, uhm. That they’re, like Ragen Chastain has a summer series where they’re going to be talking about all sorts of things related to these, are people, some of them have credentials, some of them don’t. Some of them have lived experience, some of them have a past career inside the current medical weight centric model or they did and then they left and that’s their expertise. There’s also different kinds of supervision and, and that are done by people who are speaking from a fat liberationist perspective and their expertise is that they have lived this life, right? And there’s something so invaluable about that. Like there is no textbook, there is no credentials that you can get that can come close to touching that, and so I think that’s also important. I just realized the first thing that I said were all credential things, so I also want to name things that are not. ’cause I’m on the hook. Uhh, so I meant to say that’s that’s so important.
L: Thank you for naming all those resources, Jenn.
C: Yeah, absolutely.
J: OK, let’s do some of our wrap up questions of two wonderful interviews with you.
[1:24:49]
J: We’ve talked a lot about the big and small picture perspectives in this conversation, emphasis on the big I would say. [laughs] What do you think we can all do to make a difference with what we have learned or are unlearning today?
L: I mean, my instinct initially is to, to say, meet yourself where you are. So wherever you are out there listening to meet yourself where you are and, and hold space for that with compassion. So whether it’s an unlearning or the keeping yourself on the hook or maybe letting yourself be centered for the first time and that feels really hard holding compassion and like for all of these experiences out there. Uhm, that there’s another way. There isn’t just one way to do anything in, in what makes you feel most alive. That’s what I think embodiment’s really about.
C: And that’s a journal topic already, it’s like–I, I love that, yeah.
J: I love that because when we sit with such dense information and we go so deep it can feel like there has to be like one answer there. But people can be trusted for whatever answer instinctively is showing up for them and meeting themselves where they are.
J: I love that so much. Uh, yeah, thank you so much.
C: Yeah. OK, I’m gonna–well before I ask the last question, I want to say I was thinking about you coming back on and I was super excited about it obviously, and we’ve had some really great conversations. Like I love this podcast. Everybody knows that, but you’re the only person who we were like, we can’t stop talking, let’s just have you come back. [laughs] And I think that really speaks to the space that you hold, the, umm, depth at which you speak. Also, I don’t want to speak for Jenn, but gives us the space to speak and like it’s not even like giving this space, there’s just something about you. Like I see your face and like, and here’s, here just here. It’s coming, it’s coming and I can’t stop it.
[All laugh]
C: So, I, [laughs] It so I, I really appreciate just the space that you hold. Now every time I think of you, I’m going to think of you like this like tethered balloon. What’s your favorite color? [laughs]
L: My favorite color is purple.
J: Yes! [laughs]
L: OK, but most recently it’s been a blue purple. I’m not kidding. I have, do you see my nails?
C: Yes, yes. [laughs] It’s like the crayon. The blue violet crayon.
J: Yes, yes.
C: Those look good. So it’s a, it’s a purple blue balloon, that I will see now.
J: Yes, and it’s not a competition, I’m just way too excited about favorite color. It’s not a competition.
[All laugh]
C: I love it, so thank you for that so, so thank you so much for being here with us as we finish up this episode today.
L: Thank you.
[1:28:09]
C: What would you like everyone listening to know about what you’re up to and how they can find you? And what direction do you see your career and or work taking in the future?
L: Yeah, thank you. It’s an honor to be here for a second time. I love hanging out with both of you and I think that being here is, umm, ust proof that, like being on the Internet and connecting is, is just as valuable as being in person. I really, like, you can get, you know, chills and itchy and all the feelings and emotions still come. So I’m grateful for this space. And where can people find me and what am I doing? So I’m doing a few different things. I have a private practice that’s virtual. I’m in New York City, but I am offering services internationally and, and working with people across the United States on a virtual level. And what I am offering. Uhm, let’s see, well, any sort of nutrition counseling, unlearning of sort of chronic dieting, eating disorder recovery. I also am starting to focus more on diabetes, gestational diabetes and type 1 and type 2 diabetes are also with the intersection of eating disorders, but any relationship with food and there that’s offered. And I work with gender-affirming care for trans and nonbinary folks who may be doing some sort of hormone therapy and want to work on body image healing or nutrition. I can be found at chelsealevynutrition.com as well on Instagram at Chelsealevynutrition. And I will be out there on, on the web doing my Lives and as often as I can and will be on podcasts. So keep an eye out for me. And if you’re interested in connecting it would be an honor to hear from you. Thank you.
C: Oooh, this is–
J: I’m like hugging my self-ish right now so it can–just felt the need for a hug there. Thank you for being with us.
C: Yeah, so, so much.
J: You’re the best for coming back.
C: You are. It’s always wonderful to speak with you in any area of our lives, and especially what an honor to have you here on our podcast. This has been such a gift, so again, thank you, so, so, so much?
J: Wonderful! Well, thank you for being here and we’ll see you next time.
C: Bye!
L: Thank you!
J: Thank you for listening to season 2 of the Embodiment for the Rest of Us podcast. Episodes will be published every two weeks-ish (because let’s be real here) wherever you listen to podcasts.
C: You can also find the podcast at our website, embodimentfortherestofus.com and follow us on social media, on both Twitter @embodimentus
J: And on Instagram @embodimentfortherestofus We look forward to being with you again next time in conversation.
[Music Plays]